Retinal Detachment

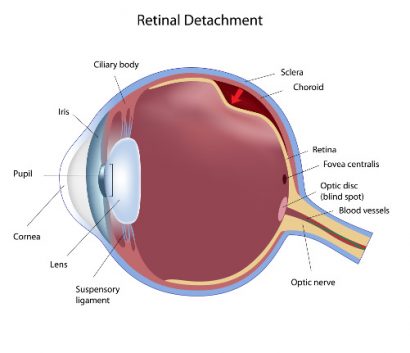
The retina is the layer of tissue at the back of the eye responsible for receiving light from the lens and transferring it to the brain via the optic nerve to make vision possible. Between the lens at the front of the eye and the retina at the back of the eye is a clear gel substance called vitreous. Vitreous is a sticky (i.e. highly viscous) gel that serves to maintain the shape and size of the eye.
Vitreous gel is not replenished, meaning that it can break down and shrink as we get older. As the vitreous shrinks, due to its sticky nature, it can pull on the retina. This process can lead to retinal detachment, an extremely serious eye condition that can result in blindness.
Causes and Risk Factors
Although shrinking vitreous is often related to retinal detachment, sometimes the vitreous can shrink without any effect on the retinal tissue. There are many other causes of detachment, because in reality, any type of activity that causes the retina to move or to be weakened can cause detachments. Some examples include:
- Trauma/injury to the face
- Extreme nearsightedness (a result of thinner, weaker retinal tissue)
- Diabetic retinopathy
- Eye surgery (in rare cases, LASIK and cataract surgery may cause retinal detachment)
You may be at increased risk of retinal detachment if you are over the age of 50, have a family history of retinal detachment or are extremely nearsighted. Also, people who engage in contact sports that can injure the face (such as boxing) are at increased risk of trauma-induced retinal detachment. If you have a pre-existing eye condition, or suffer from diabetes or sickle cell disease, you may also be at increased risk of retinal detachment.
It is important to schedule routine eye exams to evaluate eye health and determine whether you have risk factors for retinal detachment or some other eye disease. This is especially important if you begin to display any of the signs or symptoms associated with a detached retina.
Symptoms of Retinal Detachment
Retinal detachment is a serious eye condition, but fortunately there are warning signs that can help you identify the problem before it damages your vision beyond repair. Although retinal detachment is a painless condition, symptoms can include:
- Blurred vision
- Increased number of eye floaters across field of vision
- Flashes of light
- Shadow vision
- Loss of peripheral vision
If you are experiencing any of these signs, it is important that you seek medical attention as soon as possible to prevent irreversible vision loss.
Treatments for Retinal Detachment
When it comes to treating a detached retina, the only option is surgery. (The sooner, the better.) Retinal reattachment surgery should be performed by a retinal specialist or ophthalmologist with advanced training in retinal detachment.
Generally speaking, there are three surgical options for reattachment:
Scleral buckling – This is the most common surgical approach to treating retinal detachment. It involves attaching a buckle (silicone or plastic) to the outside of the eye (sclera) in order to serve as a countermeasure to detachment. The buckle compresses the eye, forcing detached retinal tissue to the back of the eye where it can reattach. The scleral buckle cannot be felt or viewed, essentially making it invisible. It is sewn to the sclera and typically left in place permanently.
Vitrectomy – If shrinking vitreous gel is the cause of retinal detachment, a scleral buckle may not be able to prevent future detachment without additional treatment. Vitrectomy surgery involves removing the gel from inside the eye and replacing it with a silicone alternative. This silicone oil will remain permanently in place and can fill the gaps created by shrinking vitreous, forcing the detached retinal tissue to the back of the eye where it can reattach. Vitrectomy also serves as a treatment for chronic eye floaters caused by pieces of the vitreous gel breaking off and “floating” around the eye.
Pneumatic retinopexy – Certain cases of retinal detachment can be corrected through an outpatient procedure called pneumatic retinopexy. A gas bubble is injected into the center of the eye which increases pressure inside the eye and forces the detached tissue back into place, where it can then be sealed using a laser (photocoagulation) or freeze probe (cryopexy). The bubble does not dissipate immediately. Instead it remains in place for one to three weeks to help hold the retina in place so that the detachment can heal fully. Patients are often asked to spend their days lying face down for seven to 10 days after the procedure, so that the gas bubble floats up in the vitreous (stays in the back of the eye) and maintains pressure on the retina to hold it in place while healing. Your doctor will also advise against air travel because the change in altitude could affect the size of the bubble, increasing ocular pressure.
Depending on the cause and complexity of your retinal detachment, your ophthalmologist or retinal specialist may recommend a combination of treatments to best correct the issue.
It’s also important to note that not all cases of retinal detachment can be treated. In some cases, excessive scarring could impede treatment efforts. Unfortunately, these cases will ultimately result in blindness. This underscores the importance of catching retinal detachment or any associated risk factors as soon as possible.
If you are at increased risk of developing retinal detachment, or if it’s been a while since you’ve undergone a comprehensive eye exam, consider scheduling a visit with an ophthalmologist for evaluation.
