Diabetic Retinopathy Treatments
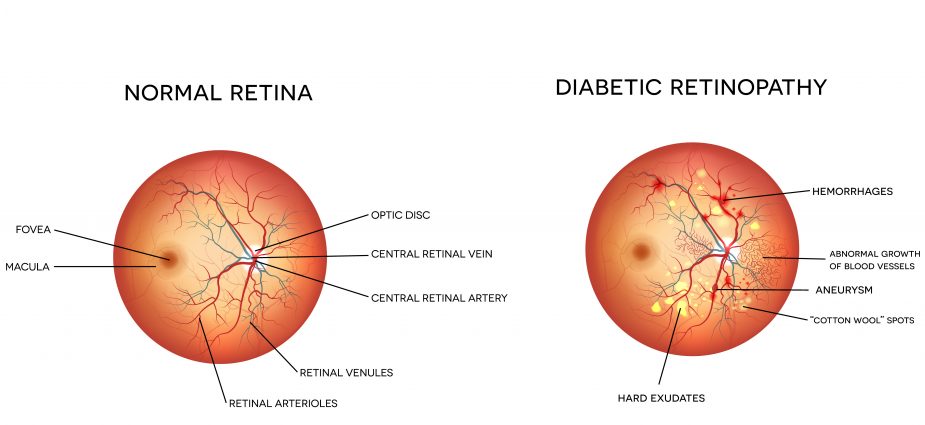
Diabetic retinopathy is the most common diabetic eye condition and the leading cause of blindness in people with diabetes, according to the National Eye Institute (NEI). The condition can occur in people with Type 1 or Type 2 diabetes, and is caused as a result of abnormal blood vessel growth on the retina (the light-sensitive tissue at the back of the eye). This is also referred to as diabetic macular edema (DME). These vessels can swell and leak fluid into the eye that can cause vision problems ranging from blurred sight to blindness.
Diabetics are at risk of a variety of health conditions associated with the disease. It is therefore incredibly important to carefully monitor blood-glucose levels and lead a healthy lifestyle in order to avoid developing associated conditions like diabetic retinopathy. As the saying goes, the best form of treatment is prevention.
Although there is no curative treatment for diabetic retinopathy, there are several that can help minimize the damage and slow the associated progression of vision loss. Your ophthalmologist will work closely with you to evaluate the severity of your condition and other unique considerations related to your health to determine the best course of treatment for you. Generally speaking there are five treatment options for diabetic retinopathy:
- Healthy Lifestyle
- Laser Treatment
- Medication Injections
- Injectable Implants
- Vitrectomy Surgery
Healthy Lifestyle
A primary treatment for diabetic eye disease targets the diabetes itself. A healthy lifestyle which maintains proper blood sugar levels can go a long way toward blunting the overall progression of diabetes, and its associated diseases like diabetic retinopathy. Your ophthalmologist can communicate with your internal medicine specialists if he or she has any questions about the treatment strategy for overall health maintenance in the face of your diabetic condition.
Laser Treatment
Laser treatments can be used to target the abnormal blood vessel growth responsible for diabetic retinopathy. Blood vessel leaks can be closed (cauterized) using targeted laser energy (photocoagulation) in some cases, or the laser may be used to target and destroy the abnormal blood vessel network. This procedure is called grid laser photocoagulation. Depending on the specific nature of your condition, laser treatment may even be used to target peripheral retinal tissue to help improve the flow of blood and the oxygen supply to the center of the retina (macula). This procedure is called panretinal laser photocoagulation. The downside of targeting peripheral retinal tissue in this way is that peripheral vision can be compromised. However this can be a small price to pay for protecting your more important central vision.
Diabetic retinopathy laser treatments are typically performed in a matter of minutes on an outpatient basis in an eye doctor’s office. Discomfort during the procedure will be minimized with a topical anesthetic or minor injection administered prior to treatment. You will need to arrange for someone to drive you home after treatment given that short-term vision may be compromised.
Although laser treatment can be effective in helping to limit vision loss caused as a result of diabetic retinopathy, it’s important to keep in mind that it usually does not improve vision.
Medication Injections
The abnormal blood vessel growth associated with diabetic retinopathy is tied to a specific protein called vascular endothelial growth factor (VEGF). There are a number of drugs that target VEGF to inhibit abnormal blood vessel growth. These anti-VEGF drugs include Lucentis and Eylea. Both are FDA approved for the treatment of diabetic macular edema.
Anti-VEGF drugs are injected directly into the retina during a simple outpatient procedure. Depending on the severity of your condition, you may require multiple injections spread over several months. These injections may be supplemented with corticosteroids which can help decrease VEGF levels and other “signal” proteins called cytokines. The combination is now often preferred over laser treatment.
Injectable Implants
In addition to anti-VEGF and corticosteroids, there is another medicated option for treating diabetic retinopathy: an implant placed inside the eye. Two injectable implants commonly used in the treatment of diabetic retinopathy are Iluvien and Ozurdex. (Retisert is another implant currently being used for the treatment of DME, though it is an “off label” use.) Their function is similar to that of other injectable medications, the difference being that these tiny implants deliver a sustained dose of corticosteroids to the retina.
Patients who have not experienced increased ocular pressure with previous injections of corticosteroids (a relatively common side effect) may be prime candidates for the implants. The sustained, slow release associated with these implants can provide for better longevity and potentially better results than more traditional single, higher-dose injections of corticosteroids.
Vitrectomy Surgery
Vitrectomy surgery represents a more invasive approach to the treatment of diabetic retinopathy. But in some cases it is unavoidable. If swelling and leaking of the blood vessels lead to bleeding and blood pooling in the vitreous (the gel-like substance between the retina and the lens of the eye) then vitrectomy surgery will likely be required to remove the blood and associated scar tissue. The blood in the vitreous blocks light entering the eye and can prevent it from being properly focused on the retina, in turn causing problems like blurred vision. By removing the hemorrhage with a vitrectomy, it can restore visual clarity. Depending on the severity of your condition, your surgeon may also perform laser photocoagulation in conjunction with vitrectomy.
In addition to causing blurred vision and preventing laser photocoagulation from being performed (it obscures the retina), a vitreous hemorrhage can also lead to retinal detachment, another serious eye condition that can lead to blindness if it is not immediately treated.
Vitrectomy surgery is also an outpatient procedure, but unlike laser photocoagulation and medication injections, it must be performed in a hospital or surgical center.
Stay Healthy and Get an Eye Exam!
If you have diabetes it is important that you closely monitor your blood-glucose level and carefully manage your dietary and lifestyle habits — for the benefit of your total health. Get into the habit of having regular eye exams with an ophthalmologist (especially if you have heightened diabetic retinopathy risk factors) so that you can best manage any development of related diabetic eye conditions.
